


For any donations…
My story continuing at:
Copyright © 2017 by Jo Barlow
Health Ombudsman Complaint -
Part 5, the final part of my complaint about my complaint to the health ombudsman!…
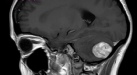
7) Dr Brodie said I had ataxia in January, and this is listed as a neurological symptom according to the NHS, and it continuing and getting worse is surely a progressive, sub‑acute loss of central neurological function? So why wasn’t I referred for a brain scan or a neurologist as urgent-
8) How can my gait be referred to as normal when I had my husband holding my arm as I walked in the room as I was so unbalanced? Especially as only Dr Brodie did a heel to toe test.
9) Re your advice from the ‘GMC’s good medical practice’, I disagree that many of these points were applied.
10) Please can Giggs Hill show me that they have ‘Significant Event Analysis Meetings’ for cases where there is a serious health concern, or rare diagnosis-
11) Why was this chart not used by Giggs Hill and a normal neurological exam deemed higher significance than dizziness or increasing and worsening headaches?
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2593538/table/tbl1/ (Table shown on part 4)
Re point 7: I am also pretty disgusted that my links and comments were supposedly read and yet you stated that your advisor found no evidence that the practice did not adhere to NICE and GMC guidance. How can these links not count? Maybe as it would mean the doctors obviously failed me if you did take them into account? The links are from medical websites, not someone’s personal opinion. If they don’t count then your guidelines need updating.
Although the NICE guidelines say “Consider an urgent direct access MRI scan of the brain (or CT scan if MRI is contraindicated) (to be performed within 2 weeks) to assess for brain or central nervous system cancer in adults with progressive, sub‑acute loss of central neurological function. [new 2015]”
I believe I did have progressive, sub-
For your information the words (on the NICE guidelines) ‘central neurological function’ do not give an exact result in Google-
How would the doctors have listed that there were abnormalities on examination if they didn’t even check? Only Dr Brodie did the heel to toe test and that was still the only hard cerebellar sign I had when I was admitted to St George’s at A&E as an urgent case. I also had plenty of other signs that I tried to tell them as many of as possible. How do I know which symptom may be relevant when you have a whole list of new issues that are getting worse by the day – and are not helped when you are told to only mention one issue by the GP! Also I was certainly not asked if I had headaches that woke me at night, felt nauseous etc. (I had lost about ½ stone in a couple of months by March 2016-
Finally, I was not aware that GPs were able to ask for direct access to scans, or I would have been pushing for that and not just seeing a neurologist to then refer me for a scan. I KNEW there was an issue with my head or neck, and as you can see I wrote these concerns down for Dr Milne as knew most of my symptoms could have been various serious problems.
Point 8: Raised in comments above. How can my gait be referred to as normal when I had my husband walking me into the room to stop me falling over? If I walked alone I would possibly bounce off the walls, chairs etc, and I always had my hands held up slightly to the sides to balance me! Dr Vo and Dr Milne also did not test my heel to toe walking, so how could they have seen if balance problems were present?
Point 9: I have already mentioned my concerns with your comment that Dr Vo acted in guidance with the GMC guidelines already in point 3 above.
Re Dr Milne-
Adequately assess the patient’s conditions, taking account of their history (including the symptoms and psychological, spiritual, social and cultural factors), their views and values; where necessary, examine the patient I do not feel this was done particularly well and there were errors that I feel Dr Milne acknowledged, plus even though she had written I was tearful and anxious I did not feel she belittled me for being that way. Although the fact I felt she understood (possibly more than she did) was why I had assumed I was getting an urgent referral and she took my condition far more seriously than I had received with Dr Vo.
Promptly provide or arrange suitable advice, investigations or treatment where necessary. I do not feel this was done, but do feel from the final reply from Glenlyn that Dr Milne recognises she did not communicate with me correctly about the referral.
Point 10. I have spoken to two NHS GPs, and a senior GP receptionist who all have told me that these Significant Event Analysis Meetings ONLY happen where the doctors didn’t diagnose correctly or made a mistake. Also on my final letter from Glenlyn it clearly states that this meeting found Dr Brodie’s actions were “considered appropriate” yet fails to mention feedback of any of my other appointments with Dr Vo or Dr Milne – which surely means they did not find the same result with either of them?
Point 11. I know I have mentioned this chart earlier and included it on my last letter to you, but all the doctors comments and your reply still seem to be saying that (even if done fully and correctly-
And of a lesser concern to my case:
12) Appointment times. You said in your final report that these could not be formally investigated as I had not raised them as a concern previously with the practice, yet I did in my complaint letters to Glenlyn on 16/11/16 “In September I booked to see a GP to go through some of my ongoing symptoms since the operation – the earliest appointment we could get was about 5 weeks later on 24th October!”
I also listed 5 separate date concerns to Charlotte Cheshire on my letter dated 17/8/17.
13) Re my referral to St Georges-
I would also like to bring up some concerns I have:
14) On my discharge letter from the Physiotherapy Department at Molesey Hospital, the information states “her symptoms have now improved significantly and she has full active range of movement (in) the neck with minimal discomfort”…which is completely opposite to what I was saying to them and untrue!
When in fact neither or the two physiotherapists I saw seemed to be able to explain why I was getting dizziness from the neck symptoms I had, I had told Kamil that when I did the exercises he set they made me feel worse-
15) I am also very concerned about the report of my NHS 111 call. The difference in what I was feeling and what was written is enormous! From the operators report it seems I presented with little more than a mild headache, from my experience I was sitting on my sofa, in blinding pain, barely able to move or put my head up or down without it feeling like it was going to explode and my eyes twitching with the severity of pain when I moved. I could barely talk or listen to them as the pain was so severe and I now think I was in some kind of shut down. This pain was FAR worse than anything I experienced in hospital after brain surgery! Even when I refused pain killers.
I know I said no to some of the things listed, but certainly not all on the listed report and I have absolutely no recollection that they told me to go to my GP within 3 days if it continued. I remember thinking at the time that this was a pointless phone call as all they did was tick off boxes and that they didn’t listen to me at all, or understand that I had a neurologist referral and my concern was could this be something serious?
The reason we called them is my husband wanted me to go to A&E, but I refused saying I couldn’t manage it and didn’t want to go. Plus, as keeps being advertised-
I would like it if someone could listen back to this recording and see if the call handler acted appropriately?
Finally on this call-
The ending of this letter was written on my first part of this blog post. I have no idea if the Health Ombudsman will even address it, or on some bureaucratic bullshit they will once again find no fault with any of the GP’s or the doctors practice. But my next step is to contact the GMC about making a complaint about two of the doctors.
The system where a patient has to complain about their treatment without support from someone who knows how to complain for them is ridiculous. As there is one thing I have learned -
But speaking as a patient who has had brain surgery-
It was only the last few months (at least 18 months after surgery) where I looked again at the reply comments and could see the instances where they had contradicted themselves in what they had written, or mentioned something that they didn’t do and I had the realisation that I needed to reply back directly to that point. Yet they are doctors who know the technical names, what the procedures are and can probably have lawyers on it right away to make sure they don't say something they shouldn’t. I was still suffering with a traumatic brain injury -
I so appreciate I was lucky. My parents paid for a private Dr, then scan. I didn’t have a stroke or anything that caused significant damage to my heath because of the delays that shouldn't have happened, despite the fact that my health was deteriorating fast. But it really was luck and privilege (or my parents giving me that privilege) that prevented anything more serious, and many people don’t have either.
It is for those other people that I will do my best to make sure that these doctors, and hopefully others will not fail other patients in the future, and urgently refer them for the treatment they deserve… the percentage of survival for brain tumour patients is dire enough as it is, the delay could easily be enough to kill them..
I really was lucky.
Next -

