


For any donations…
My story continuing at:
Copyright © 2017 by Jo Barlow
Health Ombudsman Complaint -
Part 4 of my complaint about my complaint to the health ombudsman… I have listed only a couple of the summary points at a time, so I can include my comments about them in the same blog post.
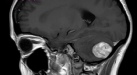
This is a long post, and involved me looking at the various guidelines in online medical sites as to what the correct response should be with someone with the symptoms I showed. It actually makes me somewhat angry and tearful as I had so many signs that the GP should have sent me for an urgent MRI (something I did not know could happen-
I also have a now friend who had the exact same tumour and operation as me, yet when she saw her GP she was sent for a CT scan THAT DAY and operated on a week later! Purely as her GP recognised the signs of a possible brain tumour-
5) I believe Dr Milne did not write down my symptoms correctly, nor understand their seriousness, and should have referred me directly to have an imaging scan.
6) Why was my ENT appointment sent as URGENT (letter dated 27th January 2016 by Dr Brodie) yet when I finally got the appointment with neurology it was not sent as urgent, despite being about the exact same problems?
Point 5: On my medical notes it states than on 23rd March 2016 Dr Milne assessed my gait as normal. How can she have done this without adequate testing? (as point 4)
She also has written that I was ‘tearful and anxious’ which from latest research suggests it would also be related to damage in my cerebellum and I feel should have been taken as yet another symptom that I had a possible issue there.
In fact I had said to all the doctors that I felt I was going insane and was super anxious and felt my ‘fight or flight’ was on overdrive-
https://en.wikipedia.org/wiki/Cerebellar_cognitive_affective_syndrome “They reported that patients with injury isolated to the cerebellum may demonstrate distractibility, hyperactivity, impulsiveness, disinhibition, anxiety, ritualistic and stereotypical behaviors, illogical thought and lack of empathy, aggression, irritability, ruminative and obsessive behaviors, dysphoria and depression, tactile defensiveness and sensory overload, apathy, childlike behavior, and inability to comprehend social boundaries and assign ulterior motives” & “Levels of depression, anxiety, lack of emotion, and affect deregulation can vary between patients”
On the letter written to referral to the neurologist, she has written “may lose her balance if turns quickly”-
She also contradicts the point that I had ‘no loss of balance’ by writing “she does fall slightly to the left with her eyes closed” in her notes.
Also I would appreciate answers to my questions in my last letter to you as I feel these all relate for certain by the last appointment with Dr Milne:
I am not sure that you are reading the same NICE guidance as me? (Nice Guidance for suspected cancer of Brain and Nervous System)
As it says Consider an urgent direct access MRI scan of the brain (or CT scan if MRI is contraindicated) (to be performed within 2 weeks) to assess for brain or central nervous system cancer in adults with progressive, sub‑acute loss of central neurological function. [new 2015]
Surely I HAD sub-
Signs and symptoms of nervous system disorders are:
The following are the most common general signs and symptoms of a nervous system disorder. However, each individual may experience symptoms differently. Symptoms may include: Persistent or sudden onset of a headache, A headache that changes or is different, Loss of feeling or tingling, Weakness or loss of muscle strength, Sudden loss of sight or double vision, Memory loss, Impaired mental ability, Lack of coordination, Muscle rigidity, Tremors and seizures, Back pain which radiates to the feet, toes, or other parts of the body, Muscle wasting and slurred speech
Of which I had: Persistent or sudden onset of a headache, A headache that changes or is different, Loss of feeling or tingling, Weakness or loss of muscle strength, loss of sight and blurry vision, Impaired mental ability, Lack of coordination, Muscle rigidity, Muscle wasting and slurred speech.
Or on: http://www.gpnotebook.co.uk/simplepage.cfm?ID=1905918027
It says to refer urgently patients with:
Symptoms related to the CNS in whom a brain tumour is suspected, including:
progressive neurological deficit, new-
Of which I had: progressive neurological deficit, headaches, mental changes, headaches of recent onset.
Accompanied by features suggestive of raised intracranial pressure: drowsiness, posture-
Or on: http://practicemattersmag.co.uk/article-
“When should a patient be referred to a Neurologist?”
It says for these symptoms how urgently they should be referred:
Upper motor neurone signs-
Cortical, cerebellar or brainstem signs: urgent (referral)
Vertigo
If accompanying earache, discharge, tinnitus or hearing loss: consider referral to ENT
If other neurological symptoms or signs: urgent referral
Which strongly suggests that I SHOULD have been referred urgently, and not at the 4th Doctor appointment, as routine.
On https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2593538/
‘Imaging patients with suspected brain tumour: guidance for primary care’ it says:
Headache with associated features
A recent review of the literature of headache with associated features found the following relevant positive likelihood ratios (likelihood ratio = post probability/prior probability) with 95% confidence intervals (95% CIs): headache with abnormal findings on clinical neurological examination 5.3 (95% CI = 2.4 to 12); headache aggravated by exertion or Valsalva-
With this table shown: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2593538/table/tbl1/
I HAD headaches causing me to wake from sleep, dizziness and lack of coordination, rapidly increasing headache frequency (from none in November 2015 to every day in March 2016), aggravated by exertion or Valsalva-
These top 3 symptoms (which I had) say they are FAR more likely than ‘abnormal neurological examination’ or ‘headache with focal neurological symptoms’ to show the risk of a tumour…yet your report seems to say that the doctors only took into account the abnormalities on neurological examination. How can these other things I had stated not be taken into account?
Recommended guidance for investigating for tumour in primary care.
• Red flags — presentations where the probability of an underlying tumour is likely to be greater than 1%. These warrant urgent investigation.
• Papilloedema
• Significant alterations in consciousness, memory, confusion, or coordination
• New epileptic seizure
• New-
• Headache with a history of cancer elsewhere particularly breast and lung
• Headache with abnormal findings on neurological examination or other neurological symptoms (although evidence base suggests orange flag)
• Orange flags — presentations where the probability of an underlying tumour is likely to be between 0.1 and 1%. These need careful monitoring and a low threshold for investigation.
• New headache where a diagnostic pattern has not emerged after 8 weeks from presentation
• Headache aggravated by exertion or Valsalva-
• Headaches associated with vomiting
• Headaches that have been present for some time but have changed significantly, particularly a rapid increase in frequency
• New headache in a patient over 50 years
• Headaches that wake the patient from sleep
• Confusion
• Yellow flags — presentations where the probability of an underlying tumour is likely to be less than 0.1% but above the population rate of 0.01%. These require appropriate management, and the need for follow-
• Diagnosis of migraine or tension-
• Weakness or motor loss
• Memory loss
• Personality change
So if I had these signs below why wasn’t I given an urgent CT scan or MRI?
Red flags:
Significant alterations in consciousness, memory, confusion, or coordination
New-
Headache with abnormal findings on neurological examination or other neurological symptoms (I could not do heel to toe test)
These orange flags:
New headache where a diagnostic pattern has not emerged after 8 weeks from presentation
Headache aggravated by exertion or Valsalva-
Headaches that have been present for some time but have changed significantly, particularly a rapid increase in frequency
Headaches that wake the patient from sleep
Confusion
And these yellow flags:
Diagnosis of migraine or tension-
Weakness or motor loss
Memory loss
Personality change
And on: http://www.nhs.uk/Conditions/Brain-
Common symptoms of increased pressure within the skull include:
new, persistent headaches – which are sometimes worse in the morning or when bending over or coughing, persistent nausea and vomiting, drowsiness, vision problems – such as blurred vision, double vision, loss of part of the visual field (hemianopia), and temporary vision loss, epileptic fits (seizures) – which may affect the whole body, or you may just have a twitch in one area
and for the cerebellum – may cause balance problems (ataxia), flickering of the eyes (nystagmus), and vomiting.
When to see your GP
It's important to see your GP if you have symptoms like those described above.
While it's unlikely that you have a tumour, these type of symptoms need to be evaluated by a doctor so the cause can be identified.
If your GP is unable to find a more likely cause of your symptoms, they may refer you to a brain and nerve specialist called a neurologist for further assessment and tests, such as a brain scan.
Or on https://www.ncbi.nlm.nih.gov/pmc/articles/PMC515188/
The reasons for a GP sending a patient for scanning with a headache.
It says it should be done for people “with symptoms suggestive of raised intracranial pressure, such as new onset headache in the early morning; or headache that is worsening with coughing, sneezing, or straining should each be viewed with concern”
Dr Brodie said I had ataxia in January, and this is listed as a neurological symptom according to the NHS, and it continuing and getting worse is surely a progressive, sub‑acute loss of central neurological function?
So why wasn’t I referred for either a neurologist or for a brain scan with 3 GP appointments and only as NON URGENT on the 4th?
Also regarding the final reply letter from Glenlyn, it clearly states that Dr Milne “did not give sufficient weight to your symptom cluster when deciding upon a routine referral” and did not clarify why she was referring me and why it was on a non-
The letter again has no comment as to what was said about this consultation at the Significant Events Analysis Meeting (again as I am assuming they did also find I should have been treated differently to how I was?)
Point 6: this has been covered in point 5 above
Next -
|
Clinical feature |
Likelihood ratio (95% CIs) |
Risk of tumour in headache presentations in primary care, % |
|
Headache causing waking from sleep |
98 (10 to 960) |
9 |
|
Dizziness or lack of coordination |
49 (3 to 710) |
4 |
|
Rapidly increasing headache frequency |
12 (3 to 48) |
1 |
|
Abnormal neurological examination |
5.3 (2.4 to 12) |
0.5 |
|
Headache with focal neurological symptoms |
3.1 (0.37 to 25) |
0.3 |
|
Aggravated by exertion or Valsalva- |
2.3 (1.4 to 3.8) |
0.2 |
|
Associated vomiting |
1.8 (1.2 to 2.6) |
0.2 |
|
Worsening headache |
1.6 (0.23 to 10) |
0.1 |

